1 Introduction: The compact control unit Morcellator with its simple and intuitive operation panel controls the speed of the attached instruments. For the morcellation of tissue speeds of up to 700 RPM are appropriate. The Morcellator attached instruments include Cutting tubes, Obturator, Trocar sleeve, Dilator, Guiding bar, Convertor, Uterine forceps. To suit the needs of every procedure the model range of the Morcellator consist of instruments with three different diameters. They are available in diameter 10, 15 and 18 mm. By carefully composed and aligned instruments and accessories the system as a whole delivers excellent results at morcellation and guarantees for maximum safety at operation.
If you are looking for minimally invasive surgery medical instruments with good quality, competitive price and reliable service. Wanhe medcal is manufaturing these for you. We provide general and professional laparoscopic instruments with CE, FDA approved.
2 Specifications 1 Adopt optimum quality stainless steel material
2 Corrosion resistant
3 Tough construction
4 Light weight and easy operation
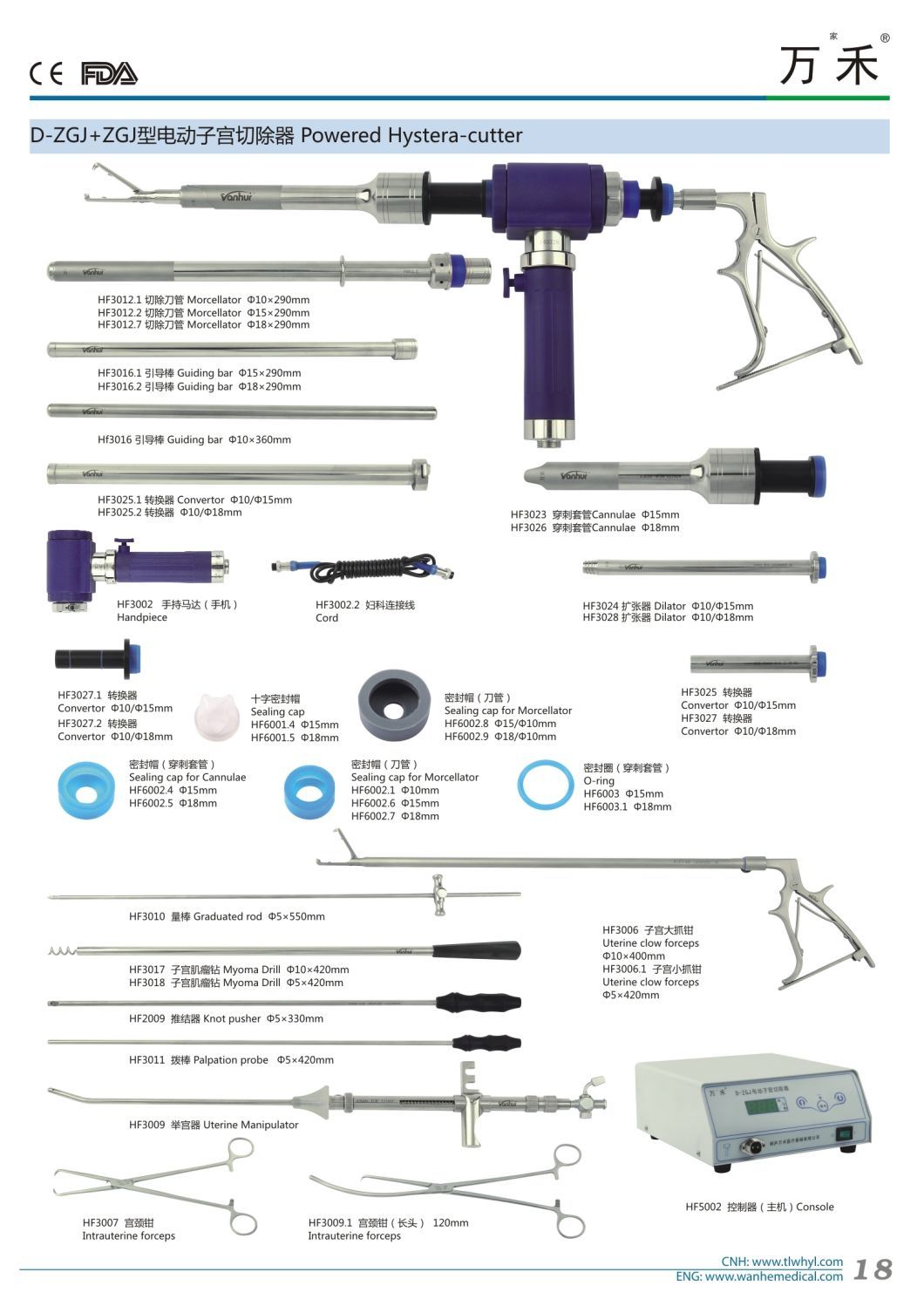
5 Fast and safe Morcellator Set For Your Reference: | Model | Name | Specifications |
| HF5002 | Morcellator Console | / |
| HF7005.2 | Handpiece/Gear unit/Handle | / |
| HF3002 | Cutting tube | Φ10x260mm |
| HF3012.2 | Cutting tube | Φ15x260mm |
| HF3012.7 | Cutting tube | Φ18x260mm |
| HF3016 | Guiding bar | Φ10x260mm |
| HF3024 | Dilator | Φ10/Φ15mm |
| HF3028 | Dilator | Φ10/Φ18mm |
| HF3023 | Trocar sleeve | Φ15mm |
| HF3026 | Trocar sleeve | Φ18mm |
| HF3025 | Convertor | Φ10/Φ15mm |
| HF3027 | Convertor | Φ10/Φ18mm |
| HF3025.1 | Convertor | Φ10/Φ15mm |
| HF3025.2 | Convertor | Φ10/Φ18mm |
| HF3027.1 | Convertor | Φ10/Φ15mm |
| HF3027.2 | Convertor | Φ10/Φ18mm |
| HF3006 | Uterine forceps large | Φ10x400mm |
| HF3006.1 | Uterine forceps small | Φ5x400mm |
| HF3016.1 | Obturator | Φ15x260mm |
| HF3016.2 | Obturator | Φ18x260mm |
 3 Packing & Shipping:
3 Packing & Shipping: | Package detail: | Poly bag and special shockproof paper box. |
| Delivery detail: | By air |
4 Company Show






FAQ
Which patients are suitable for minimally invasive gynecological surgery?
Comprehensive management of menopause in women
American Society for Reproductive Medicine Laparoscopy and Hysteroscopy Patient Guidelines
Patients suitable for minimally invasive gynecological surgery mainly include the following categories:
Low-risk cervical cancer patients: For low-risk cases such as small cervical lesions, good differentiation, and no deep stromal infiltration, minimally invasive surgery can be chosen. Although there is currently insufficient evidence to clearly define the risk factors that affect the outcome of minimally invasive surgery for tumor treatment, these low-risk cases are the main indications for minimally invasive surgery.
Patients with uterine fibroids: Especially those with fibroids less than 3 cm in diameter, MHT (percutaneous minimally invasive surgery) can be routinely used for treatment. In addition, for older women who suffer from gynecological diseases and are eager to prepare for pregnancy, hysteroscopy combined with single-port laparoscopic myomectomy can make them beneficiaries, because this surgical method is less invasive, has a fast postoperative recovery, and can start preparing for pregnancy in the shortest time.
Patients with ovarian cancer, fallopian tube cancer and primary peritoneal cancer: Some patients can choose minimally invasive surgery for surgical staging and tumor reduction, which is used to evaluate whether satisfactory tumor reduction can be performed and whether recurrent lesions can be removed, etc., but it must be performed by experienced gynecological oncologists.
Patients with infertility: Laparoscopic surgery has a high detection rate in the treatment of female infertility and has a good postoperative recovery effect, so it is also suitable for this type of patients.
Patients with other gynecological diseases: including but not limited to uterine ligament repair, uterine laceration suture, uterine fistula closure, etc.
. Minimally invasive surgery has been widely used in clinical practice due to its advantages such as less trauma, less bleeding, less postoperative pain, faster recovery and less scar after healing.
In short, patients suitable for minimally invasive gynecological surgery are mainly those with relatively low-risk conditions, who need rapid recovery or have special needs (such as preparing for pregnancy). At the same time, it must be emphasized that all patients who choose minimally invasive surgery should be operated by doctors with relevant qualifications and experience under the premise of full informed consent.
What are the latest technologies and methods for minimally invasive gynecological surgery?
The latest technologies and methods for minimally invasive gynecological surgery include the following:
Transumbilical single-port laparoscopic surgery (TU-LESS): This technology was approved by the American Natural Laparoscopy Association in 2009 and recommended for use by the Chinese Medical Association Surgery Branch. It has broad application prospects in gynecological surgery, such as adnexa, uterus, pelvic adhesion lysis and pelvic organ prolapse surgery. Its advantages are clear surgical field, convenient operation, less bleeding, beautiful postoperative incision and fast recovery.
Da Vinci Robotic System: This system is one of the most advanced minimally invasive technologies. It has a 3D high-definition imaging system, a vibration filtering system and a flexible arm-wrist structure, which can effectively break through the limitations of traditional laparoscopic surgery. Despite its disadvantages such as high cost and lack of tactile feedback, it has broad application prospects in the treatment of benign and malignant gynecological diseases.
Trans single-port laparoscopic surgery (V-NOTES): This technology is performed through the , with less trauma and faster recovery. It is suitable for complex operations such as total hysterectomy and adnexa, and has been carried out in some hospitals.
High-intensity focused ultrasound ablation (HIFU knife): This is a non-invasive treatment method mainly used to treat benign tumors such as uterine fibroids. The HIFU knife uses high-intensity focused ultrasound to act directly on the lesion area without cutting the skin or tissue, and the trauma is minimal.
Comprehensive nursing intervention: Modern minimally invasive surgery emphasizes operating under the optimal internal environment of the body to achieve minimal tissue damage and the most ideal scar healing effect. Research on the application of comprehensive nursing intervention in gynecological minimally invasive surgery has shown that this method can significantly reduce patients' pain and shorten recovery time.
Cold knife hysteroscopic surgery: This technology is mainly used for the diagnosis and treatment of diseases such as endometriosis and adenomyosis. Cold knife hysteroscopic surgery has the advantages of less trauma and faster recovery.
Robot-assisted surgery platform: In addition to the da Vinci robot system, there are other robot platforms such as REVO-I and Senhance. These platforms further improve the safety and accuracy of surgery by improving the reusability of surgical instruments and adding functions such as tactile feedback.
3D printing technology combined with robotic surgery: In the future, 3D printing technology may be combined with robotic surgical systems to replace traditional patch materials to complete the surgery, which will greatly improve the personalization and accuracy of the surgery.
What are the long-term complications and risk assessment after minimally invasive gynecological surgery?
Minimally invasive gynecological surgery, such as hysteroscopy and laparoscopy, although less traumatic and faster recovery, still has certain long-term complications and risks. The following are common complications of these surgeries and their assessment:
Bleeding: This is one of the common complications in hysteroscopy and laparoscopy. Secondary bleeding or pelvic bleeding may occur after surgery and need to be treated in time.
Infection: Including surgical site infection (such as incision infection) and pelvic infection. Infection not only affects postoperative recovery, but may also cause serious health problems.
Adhesions: Uterine adhesions may occur after hysteroscopy, which will affect the function of the uterus and may lead to reoperation.
Air embolism and air embolism: In hysteroscopy, when carbon dioxide gas is used to expand the uterus, if the gas enters the vascular system, it may cause air embolism, which in turn causes pulmonary effusion and other serious complications.
Deep vein thrombosis and pulmonary embolism: Due to factors such as long-term bed rest and anesthesia, patients are prone to deep vein thrombosis, which in turn leads to pulmonary embolism and endangers life.
Urinary retention and bladder injury: Urinary retention may occur after laparoscopic surgery, and damage to the bladder during surgery may also lead to problems such as urinary incontinence.
Psychological stress: Psychological stress after surgery is also an issue that cannot be ignored. Some patients may experience negative emotions such as tension and anxiety, which have an adverse effect on postoperative recovery.
Other complications: including intestinal obstruction, lymphedema, uretero fistula, etc. These complications may require further treatment and management.
In order to reduce the risk of these complications, the patient's underlying disease needs to be evaluated in detail before surgery, and the appropriate anesthesia method should be selected; vital signs and blood gas analysis should be closely monitored during surgery, and operations should be standardized to prevent infection; postoperative care should be strengthened, pain, nausea and vomiting and other symptoms should be dealt with in a timely manner, and regular follow-up should be conducted to detect and deal with potential problems early.
How to choose the appropriate type of minimally invasive gynecological surgery according to the patient's specific situation?
Choosing the appropriate minimally invasive gynecological surgery type requires comprehensive consideration of the patient's specific situation, including disease type, severity of the disease, age, fertility needs, and personal health status. The following is a detailed description of how to choose the appropriate minimally invasive gynecological surgery type based on the information I searched:
Disease type and stage:
For early endometrial cancer (such as stage I adenocarcinoma or undifferentiated carcinoma), the preferred minimally invasive surgery is laparoscopic-assisted hysterectomy.
If the patient has high-risk factors, such as large tumors, special tissue types, or preoperative biopsy indicating vascular involvement, laparotomy is recommended.
Tumor location and size:
The size and location of uterine fibroids are important factors in determining the surgical approach. For single, subserosal or intramural fibroids with a diameter of less than 7 cm, modified laparoscopic myomectomy can be used.
For low-risk cases with small, well-differentiated cervical lesions and no deep stromal infiltration, minimally invasive surgery can be selected; for high-risk cases, such as large lesions and special tissue types, laparotomy is recommended.
Patient's age and fertility needs:
Ovarian preservation is recommended for premenopausal women under 45 years of age without obvious ovarian or other peripheral diseases.
If the patient wishes to preserve fertility, laparoscopic endometrial resection or myomectomy can be considered.
Surgical route and technical selection:
Laparoscopic surgery has the advantages of clearer vision and less trauma, and is suitable for minimally invasive surgery for most gynecological malignancies.
Robotic-assisted laparoscopic surgery is also a good choice, especially for complex cases, but attention should be paid to equipment and technical requirements.
hysterectomy is suitable for patients with poor health who cannot withstand extensive surgical procedures.
Preoperative evaluation and preparation:
A comprehensive evaluation should be performed before surgery, including family history, general evaluation and comorbidity history, geriatric assessment (if appropriate), clinical examination (including pelvic examination), and imaging examinations (such as or rectal ultrasound or pelvic magnetic resonance imaging).
For patients with multiple medical problems, if their health is not good enough to undergo extensive surgical procedures, hysterectomy can be selected.
Tumor-free operation principle:
The principle of "tumor-free operation" must be strictly followed in minimally invasive surgery to reduce the risk of postoperative recurrence. This includes measures such as improving the method of lifting the uterus, closing the below the tumor, and timely placing the specimen bag.
In short, choosing the appropriate type of minimally invasive gynecological surgery requires comprehensive consideration of factors such as the patient's specific condition, disease stage, age, and fertility needs, combined with the doctor's professional judgment and experience.
What are the results of a comparative study between minimally invasive gynecological surgery and traditional laparotomy in postoperative recovery and quality of life?
According to multiple studies and clinical analyses, the results of a comparative study between minimally invasive gynecological surgery and traditional laparotomy in postoperative recovery and quality of life are as follows:
Incision and pain:
The incision of minimally invasive surgery is usually controlled within 0.5 to 1 cm, leaving basically no scars, while the incision of traditional laparotomy is larger, usually more than 10 cm, which affects the appearance and easily leaves long linear scars.
Minimally invasive surgery uses intravenous anesthesia, and the patient completes the surgery while sleeping, with less postoperative pain. Traditional laparotomy requires laparotomy, and the postoperative incision site is often accompanied by pain, and complications such as tissue infection may occur due to the large incision.
Recovery time and hospital stay:
The recovery time for minimally invasive surgery is shorter, and patients can generally be discharged from the hospital in 3 to 5 days, and can get out of bed and move around 6 to 8 hours after surgery, and their eating conditions are relatively normal.
In contrast, the recovery time for traditional laparotomy is longer, and it usually takes 7 to 15 days to be discharged from the hospital.
Bleeding and complications:
Minimally invasive surgery causes almost no bleeding, which reduces damage to organs and functional interference, and reduces the risk of postoperative complications.
However, traditional laparotomy causes large bleeding, and is prone to problems such as incision infection or fat liquefaction.
Quality of life:
Although most studies have shown that minimally invasive surgery is superior to traditional surgery in terms of trauma, pain, recovery speed and bleeding, some studies have pointed out that in certain specific cases (such as cervical cancer), the disease-free survival rate and overall survival rate of the minimally invasive surgery group are significantly lower than those of the laparotomy group. This suggests that minimally invasive surgery may not be as good as traditional laparotomy in terms of long-term survival rate.
Economic cost:
The total cost of minimally invasive surgery is relatively low because it reduces hospital stay and the incidence of complications.
Minimally invasive gynecological surgery is superior to traditional laparotomy in terms of postoperative recovery time, pain, hospital stay and blood loss, and is a safer and more effective treatment option.
For patients with infertility, what are the latest studies on the success rate and treatment effect of minimally invasive gynecological surgery?
In recent years, with the increasing incidence of infertility, minimally invasive gynecological surgery has made significant progress in the treatment of the disease. The following is the latest research on the success rate and treatment effect of minimally invasive gynecological surgery:
Hysteroscopy and laparoscopy combined surgery is one of the important means of treating infertility. Data from Minhang District Central Hospital showed that the pregnancy rate of patients treated with hysteroscopy and laparoscopy reached 50%, which significantly improved the efficacy and increased the patient's chance of pregnancy.
In addition, the Hebei Provincial Science and Technology Research Achievement Bulletin also confirmed that hysteroscopic surgery combined with Chinese medicine enema, Danshen injection enema and oral Chinese medicine for tubal obstructive infertility can effectively regulate blood rheology, improve the patency of the fallopian tube, and have a more significant therapeutic effect.
Laparoscopic surgery is of great value in the treatment of female infertility. A study based on clinical analysis and surgical effect evaluation of 100 patients showed that after the fallopian tube dredging surgery, the patients were already patency in the second month of follow-up, with a 100% success rate. After 1 year of follow-up after the operation, 30 patients became pregnant, and the pregnancy rate reached 30%. This shows that laparoscopic surgery can improve the infertility pregnancy rate of patients.
Robotic laparoscopic surgery is superior to traditional laparoscopic surgery in some aspects. Nezhat et al. conducted a controlled trial of robotic laparoscopic and traditional laparoscopic surgery on 78 patients with deep endometriosis. The results showed that except for the longer duration of robotic laparoscopic surgery, there was no significant difference in other data between the two groups. This suggests that robotic laparoscopic surgery may have more advantages in dealing with complex cases.
Studies on the treatment of tubal obstruction infertility with minimally invasive surgery combined with comprehensive Chinese medicine have shown that hysteroscopic surgery combined with Chinese medicine enema, Danshen injection enema and oral Chinese medicine treatment can effectively improve the patient's blood rheology-related indicators and increase the patency of the fallopian tube, thereby achieving better treatment results.
Minimally invasive gynecological surgery is increasingly used in the treatment of infertility, and its success rate and treatment effect are also constantly improving. Through hysteroscopic and laparoscopic combined surgery, robotic laparoscopic surgery and combined with comprehensive Chinese medicine therapy, the patient's conception rate and pregnancy rate can be significantly improved, and the patient's physical and mental pain and economic burden can be reduced.
For more photos and details please contact me:
Company Name: Tonglu Wanhe Medical Instruments Co., Ltd.
Sales: Sue