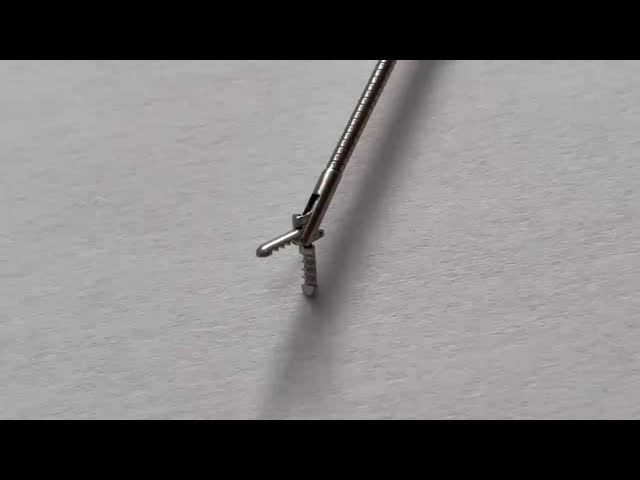
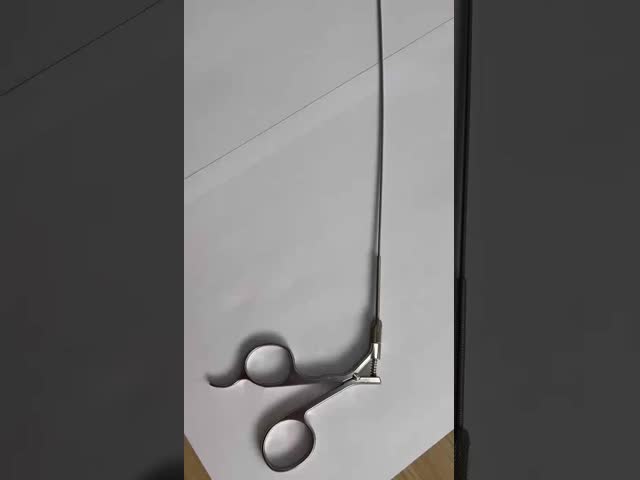
Cystoscopy Endoscope Bridge for Single Channel Biopsy Forceps Customized Request

1 Introduction:
If you are looking for minimally invasive surgery medical instruments with good quality, competitive price and reliable service. Wanhe medical is manufaturing these for you. We provide general and professional laparoscopic instruments with CE, FDA approved.
2 Specifications
Adopt optinum stainless steel material
Corrosion resistant
Tough construct
Superb workmanship
3 Various Type For Your Reference
| Model | Name | Specifications |
| HA1106.1 | Endoscope bridge | single channel |
| HA1106.2 | Endoscope bridge | double channel |
| HA1106.3 | Endoscope bridge | without valve |
| HA1204 | Endoscope bridge
(For pediatric/children urethro-cystoscope) | without valve |
4 Packing & Shipping:
| Package detail: | Poly bag and special shockproof paper box. |
| Delivery detail: | By air |
FAQ
What are the postoperative complications and risk management of urological surgical instruments?
Postoperative complications and risk management of urological surgical instruments is a complex and multifaceted topic involving multiple types of surgery and different complications. The following is a detailed analysis of this issue based on the data:
1. Common postoperative complications
Complications of laparoscopic surgery:
Subcutaneous emphysema: This is the most common mild complication in laparoscopic surgery, which usually does not require treatment and can be absorbed and disappear on its own.
Incision infection: This complication needs to be treated in time to prevent further infection.
Peritoneal tear: It is also a common complication and needs to be repaired in time when discovered.
Vascular injury: Including large blood vessel injury, such as injury to the distal end of the abdominal aorta, the inferior vena cava and its branches, the overall incidence is 0.5% to 3.0%, which is a more serious complication.
Open surgery complications:
Adrenal open surgery: It may damage surrounding organs, such as the intestines and blood vessels.
Open radical prostatectomy: It may damage the sigmoid colon and the retropubic vascular plexus.
Other common complications:
Postoperative urinary tract infection: This is a very common complication in urological surgery. The patient's body temperature, redness, swelling, pain and drainage need to be closely monitored, and these signs should be reported to the doctor in a timely manner.
Thrombosis: Such as deep vein thrombosis (DVT) and pulmonary thromboembolism (PE), is one of the common complications of the perioperative period.
Metabolic complications: Such as salt loss syndrome and metabolic acidosis.
Bladder stones, urethral/rectal stenosis, spontaneous rupture, hernia and fistula, etc.
2. Risk management and preventive measures
Preoperative preparation and evaluation:
Perform a detailed physical examination to ensure that the patient has no clear surgical contraindications, such as oral anticoagulant use and previous surgical history.
Prepare specific surgical tools and materials, such as vascular repair tools, and fully train medical staff to deal with various unexpected situations.
Postoperative management and care:
Medical institutions should do a good job in postoperative transfer connection, immediate evaluation, recovery management and discharge guidance, and eliminate postoperative safety hazards as much as possible.
Preventive measures such as using non-absorbable sutures, regularly flushing the catheter, and maintaining intestinal patency were used to reduce the occurrence of complications.
Complication care was used for patients in the observation group, and the results showed that the incidence of postoperative complications was low, the incision pain score and hospitalization time were significantly reduced, and the quality of life score was high.
Treatment of special complications:
For vascular injury, rapid transfer to open surgery for treatment.
For ureteral injury, suture or anastomosis is required to restore the continuity of the ureter.
For massive bleeding, transurethral resection syndrome (TURS), urethral stricture syndrome, etc. in TURP surgery, corresponding preventive and therapeutic measures should be taken.
Conclusion
There are many types of postoperative complications of urological surgical instruments, ranging from mild subcutaneous emphysema to severe vascular injury. Through strict preoperative preparation, meticulous postoperative management and effective nursing intervention, the incidence of these complications can be significantly reduced and the quality of patient prognosis can be improved. Medical institutions should strengthen postoperative risk management and improve the safety management system to ensure the safety and recovery of patients.
What is the latest treatment for subcutaneous emphysema in urological surgery?
In urological surgery, the latest treatments for subcutaneous emphysema include the following:
Continuous low-flow oxygen inhalation: This method can help patients dissipate subcutaneous emphysema. The specific operation is to insert a single-hole oxygen inhalation tube into the nasal cavity for low-flow oxygen inhalation, and the insertion depth is about 0.5~1cm to avoid discomfort and narrow exhalation channel.
Subcutaneous exhaust method: At each dressing change, use the palm of the hand to press the subcutaneous emphysema to drive away the gas.
Pause the operation and release the pneumoperitoneum: For severe subcutaneous emphysema, the operation can be temporarily stopped and the pneumoperitoneum can be released to reduce the occurrence of subcutaneous emphysema.
Single-lung ventilation: In retroperitoneal laparoscopic surgery in urology, the use of single-lung ventilation can significantly reduce the incidence and degree of subcutaneous emphysema. Compared with double-lung ventilation, the CO2 absorption of the single-lung ventilation group is reduced, thereby effectively controlling subcutaneous emphysema.
How to effectively prevent and manage bleeding risks after open radical prostatectomy?
How to effectively prevent and manage bleeding risks after open radical prostatectomy requires comprehensive consideration of multiple measures. The following are detailed prevention and management strategies:
Preoperative evaluation and preparation:
Perform a comprehensive preoperative evaluation of the patient, including an assessment of bleeding risk. Decide whether to stop anticoagulant therapy or bridging therapy based on the evaluation results.
Attach importance to psychological care, guide functional exercises to adapt to postoperative conditions, strengthen dietary adjustments and intestinal preparation to reduce bleeding during surgery.
Choose the appropriate surgical method:
Consider using laparoscopy or robot-assisted laparoscopy for radical prostatectomy, which has the advantages of small surgical incisions, low bleeding, and low incidence of postoperative complications.
Intraoperative operation skills:
During the operation, damage to blood vessels should be avoided as much as possible to reduce bleeding. For patients with medium and high risks, it is recommended to take more cautious operations during surgery.
Postoperative management:
Postoperatively, fluid replacement and volume expansion and anti-infection treatment should be actively performed, and blood transfusion should be given if necessary. Most minor bleeding can be improved with conservative treatment.
Pay attention to strengthening the monitoring of vital signs, maintaining the patency of each drainage tube, and promptly dealing with possible rectal injuries.
Routine fasting and abstinence from drinking for 2 to 3 days, which can be appropriately extended for suspected rectal injuries.
Drug and mechanical preventive measures:
Adjust the intensity of preventive measures according to the patient's bleeding risk level. For patients with medium and high risk, mechanical preventive measures are recommended until discharge; for low-risk patients, drug or mechanical preventive measures are not recommended.
Use retrievable filters to prevent venous thromboembolism (VTE), and regularly evaluate the removal of filters within one month after surgery.
Long-term monitoring and follow-up:
Continue anticoagulation therapy based on the risk of bleeding and thrombosis after surgery, and follow up regularly to ensure that the patient recovers well.
What are the early identification and treatment strategies for deep vein thrombosis (DVT) after urological surgery?
The early identification and treatment strategies for deep vein thrombosis (DVT) after urological surgery include the following aspects:
Before surgery, it is key to assess the risk of deep vein thrombosis in patients. This includes considering factors such as the patient's age, underlying health conditions (such as cardiovascular disease, diabetes, obesity, etc.), the type of surgery to be performed and its duration, and the ability to move after surgery. By comprehensively considering these factors, medical staff can accurately determine the patient's specific risk level of DVT after surgery and formulate corresponding preventive measures.
In the case of suspected DVT, ultrasound examination of the lower extremities and pelvic veins should be performed immediately. This is because after urological surgery, prostate cancer surgery and re-implantation of the renal pelvis may increase the risk of DVT.
Treatment methods:
Anticoagulation therapy: This is one of the most commonly used treatments for DVT, especially when DVT is suspected or confirmed, anticoagulation therapy is needed immediately to prevent blood clots from breaking off and causing pulmonary embolism.
Mechanical thrombectomy: Including percutaneous mechanical thrombectomy (PMT), this method is faster and more effective than catheter-directed thrombolysis (CDT).
Thrombolytic therapy: The use of drugs to dissolve blood clots is suitable for acute and subacute central and whole-limb DVT of the lower extremities.
Other interventional methods: such as filter implantation, balloon dilatation, stent implantation and thrombus aspiration.
In some cases, TED hoses and sequential compression devices can be used to relieve DVT symptoms and reduce the risk of blood clots breaking off.
Establish a risk warning nursing team, organize regular systematic training and learning for all members, conduct deep vein thrombosis risk assessment for each patient, and implement targeted preventive measures based on the assessment results.
What are the new prevention and management measures for metabolic complications after urological surgery?
There are currently a variety of new prevention and management measures for metabolic complications after urological surgery. These measures are aimed at reducing the patient's postoperative stress response, improving the body's internal environment, and optimizing the patient's nutritional status, thereby promoting postoperative recovery.
Whole-course nutritional management model: This model helps patients recover and treat diseases after surgery by reducing the patient's postoperative stress response and improving the body's internal environment, while improving the patient's nutritional status.
Accelerated recovery after surgery (ERAS): This program emphasizes a series of standardized nursing measures before, during, and after surgery, including stopping the use of drugs that may cause complications such as vascular endothelial growth factor (VEGF) inhibitors, cyclophosphamide, etc., and avoiding the use of drugs that may cause nephrotoxicity such as high-dose cisplatin and micafem. In addition, sodium sulfate is recommended to prevent nephrotoxicity, and granulocyte colony-stimulating factor (GCSF) is avoided to prevent moderate to severe anemia.
Blood sugar management and fluid management: For patients with diabetes, blood sugar control is particularly important after surgery. Maintaining blood sugar at 110 mg/dL or below can significantly reduce the incidence of mortality and sepsis. Therefore, blood sugar needs to be closely monitored and corresponding prevention strategies should be taken after surgery.
Monitoring and management of dyslipidemia: For renal transplant patients, blood lipid levels should be monitored from the perioperative period, and individualized blood lipid management strategies should be formulated according to the degree of metabolic abnormalities. This includes regular urine protein checks and increased testing frequency based on family history and ASCVD.
Prevention of urinary tract infection and other catheter-related complications: Long-term indwelling catheters may lead to urinary tract infections, purple urine bag syndrome, catheter obstruction and other problems. Therefore, effective management measures need to be taken, such as regular replacement of catheters, keeping catheters clean and dry, etc.
Early diagnosis and treatment: For serious complications such as bladder perforation and bacterial infection, early diagnosis and timely treatment are essential. In addition, attention should be paid to the risk of vitamin B12 deficiency, which may be associated with the removal of the small intestine and may last for many years.
How to quickly and accurately assess and manage the risk of vascular injury in urological surgery?
In urological surgery, it is crucial to quickly and accurately assess and manage the risk of vascular injury. The following is a detailed description of how to do this based on the data:
Application of diagnostic tools:
Duplex ultrasound and CT angiography are commonly used diagnostic methods that can effectively identify vascular injuries.
For large abdominal vascular injuries, open surgery is recommended, and the damaged blood vessels are sutured through the abdominal wall using straight needles.
Intraoperative monitoring and evaluation:
Closely monitor the inflow and outflow of perfusion fluid to ensure early identification of fluid overflow.
Evaluate serum electrolytes, acid-base balance, oxygenation, and monitor airway pressure, which can help detect possible complications early.
Use oxygenation pressure increased to 20-25mmHg, and insert additional puncture needles as needed, while using sponges or bandages to apply pressure to the injury site.
Postoperative management:
The patient's condition should be closely monitored in the early postoperative period, including heart rate, blood pressure and level of consciousness, and the bruises, bleeding volume, pain, etc. in the abdomen should be observed.
It is necessary to pay attention to postoperative bleeding and blood transfusion, and take necessary intervention measures in time.
Graded treatment strategy:
Different treatment plans are formulated according to the patient's stability and specific manifestations. For example, for unstable patients, immediate laparotomy or emergency treatment may be required; while for stable patients, observation and selective vascular embolization can be performed.
For visible hematuria, contrast-enhanced spiral CT scan is recommended, and the need for further angiography and selective vascular embolization is determined based on the results.
Precautions:
When performing laparoscopic surgery, hasty operations and improper anatomical identification should be avoided to reduce the incidence of vascular injury.
Use appropriate instruments and techniques, such as monopolar or bipolar electrocoagulation, to effectively close the blood vessels.
Special case treatment:
For persistent bleeding, enlarging hematoma or central hematoma caused by penetrating renal injury or blunt injury, direct evaluation is required and the need for nephrectomy is decided based on the specific situation.
Ureteral injuries are usually caused by penetrating trauma and must be suspected with imaging studies to avoid missing the diagnosis.
For more photos and details please contact me:
Company Name: Tonglu Wanhe Medical Instruments Co., Ltd.
Sales: Emma
Tel:+86 571 6991 5082
Mobile: +86 13685785706